Frequently Asked Questions
To help you answer questions related to our organization, the services we provide, and general information about the Health Insurance Marketplace, please see the FAQ below.
For additional questions not answered here, please contact us.
Under the Affordable Care Act, Health Insurance Marketplace plans must cover treatment for pre-existing medical conditions. No insurance plan can reject a user, charge more, or refuse to pay for essential health benefits for any condition one had before coverage started. Once a person is enrolled, the plan cannot deny coverage or raise rates based only on health.
Most people sign up for Health Insurance Marketplace coverage during the open enrollment period near the end of the year. Outside of that window, a small number of people meet stricter deadlines to sign up for a special enrollment period.
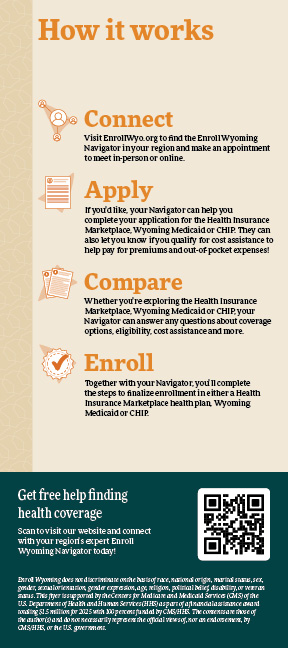
For free assistance, visit EnrollWyo.org or call (307) 996-4797 or 211.
Enroll Wyoming is supported by the Centers for Medicare and Medicaid Services (CMS) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $1.5 million for 2025 with 100 percent funded by CMS/HHS. That means Enroll Wyoming provides expert, objective information without sales incentives or quotas.
Different health plans offer different benefits, but the essential health benefits covered by every plan in the Health Insurance Marketplace are:
- Outpatient care
- Emergency services
- Treatment while hospitalized
- Pregnancy, maternity, and newborn care
- Pediatric services
- Mental health and substance use disorder services
- Prescription drugs
- Services and devices to help with recovery in cases of injuries, disabilities, or chronic conditions Laboratory tests
- Preventive and wellness services
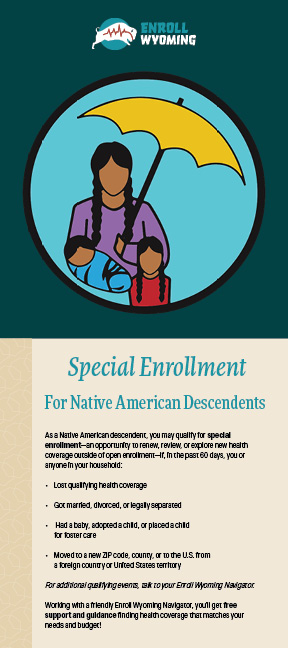
Enrolled members can apply anytime throughout the year. Depending on their income, members of federally recognized tribes may be eligible for a zero cost-sharing plan, which means that there are no additional out-of-pocket costs other than the monthly premium.
- Login/password for Health Insurance Marketplace application
- Social Security numbers for all household members applying for coverage Income information for all household members
- Employer information for all household members
- Home and/or mailing addresses for all household members applying for coverage Information on how you will be filing your taxes next year
- Heath coverage information (such as current physicians and/or drug prescriptions along with dosages)
- Citizenship/immigrant document information
- Personal information that may be needed for identification verification such as a driver’s license or other proper form of ID For in-person appointments
- If applicable, documentation of an event that qualifies you for a special enrollment period such as a marriage certificate or job termination letter.
It is helpful if you can access your email from a mobile device so you can verify login information.
A Certified Application Counselor is a person who goes through the same training as a Navigator to help people better understand health coverage and access the Health Insurance Marketplace.
A Certified Application Counselor Designated Organization, or CDO, is a group that helps individuals and families navigate enrollment through the Health Insurance Marketplace. They train staff and volunteers to provide free, unbiased assistance to your community, organization, and consumers. The training is the same that Enroll Wyoming Navigators receive.
This work helps patients, clients, and neighbors access affordable health coverage; and strengthen an organization’s role and reach as a trusted community resource.
Navigators are Wyoming residents trained to assist those in the Equality State renew, review, and explore new health coverage. They help people navigate the Health Insurance Marketplace and Wyoming Medicaid/Children’s Health Insurance Program. Navigators serve all 23 counties and offer services free of charge.
Navigators customize each consultation based on the needs and the priorities of the people they work with, so they can answer specific questions, provide related information, and identify resources so people can make informed decisions.
The premium tax credit helps eligible individuals and families pay the premiums for health coverage purchased through the Health Insurance Marketplace. To get this credit, users must meet certain requirements and file a tax return with Form 8962.
Enhanced Premium Tax Credits were created in 2021 that allowed more people to access the Marketplace at a lower cost, but without Congressional action they will end in 2025 and not be available next year. To see an estimate of what plans will cost in 2026, use this link.
We are a grant-funded, nonprofit organization designed to help Wyoming individuals, families, and small businesses explore their health coverage options. We assist people in their efforts to find, understand, or enroll in health coverage.
Open enrollment is a designated time each year when people can renew existing coverage, change health plans, or enroll in new coverage. Even those with a plan they like are encouraged to review their coverage in case there were major changes or the plan is no longer offered.
A special enrollment period (SEP) is a time outside of the yearly open enrollment period that allows people to change or add Marketplace coverage from due to a qualifying life event.These may include losing job-based health insurance; marriage; divorce; birth/adoption; death; becoming a U.S. citizen; return from military; release from incarceration; and loss or denial of government health care programs like Medicaid, CHIP, or COBRA.
The Health Insurance Marketplace is a place where people can apply for health insurance and tax credits to lower monthly premium costs. The health plans featured on the marketplace cover essential benefits. Most people can apply for marketplace coverage through Open Enrollment, though some people will qualify for Special Enrollment.
To be eligible to enroll in health coverage through the Health Insurance Marketplace, you must live in the United States; be a U.S. citizen, U.S. national, or lawfully present non-citizen; and not be incarcerated.
If you have Medicare coverage, you cannot enroll in a Marketplace health or dental plan. Just because you qualify for the Marketplace, it does not necessarily mean you will qualify for tax credits or other cost-saving benefits.